GM case
- Get link
- X
- Other Apps
32yr old male with fever and headache
32 yr old male with fever and headache
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
A 32yr old male was brought to casualty with --fever since 1 week.
-Headache since 5 days
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 1 week back. Then he developed fever which is moderate to high grade, intermittent ( on and off). He visited a local RMP and took medication. There was mild relief of symptoms.
Since 4 days he is having continous high grade fever which was not subsiding with medication.
Fever was associated with headache which was diffuse in nature and not associated with photophobia or vomitings.
Patient also has body pains since onset of fever.
The fever was not associated with:
-chills and rigors
-vomitings
-loose stools
-burning micturition
-rash
-cold,cough
-Abdominal pain
-any bleeding manifestations (malena, hemoptysis, hematemesis)
- SOB, pedal edema, bowel disturbances
PAST HISTORY:
No h/o of similar complaints in the past.
Not a k/c/o DM, HTN, thyroid, asthma, TB, CAD and, CVA.
PERSONAL HISTORY
Diet-mixed
Appetite-reduced
sleep - disturbed
bowel and micturition - normal
No addictions
No known drug and food allergies
FAMILY HISTORY:
insignificant
GENERAL EXAMINATION :
-Patient is conscious, cooperative and coherent.
-moderately built and moderately nourished.
-No pallor, icterus, cyanosis, clubbing, generalised lymphadenopathy or generalised edema
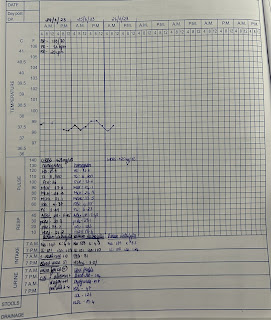
-Vitals:
Temp - 101F
PR-81 bpm
BP - 110/70 mmHg
Spo2 - 99%.
RR - 21 CPM
SYSTEMIC EXAMINATION:
-CVS - S1 S2 + no murmers heard
-RS - BAE +, CLEAR, NVBS.
-P/A - soft, non tender, no organomegaly.
-CNS - NAD
-there were multiple irregular hypopigmented lesions in the upper left side of chest
-they were not associated with itching and loss of sensation.
PROVISIONAL DIAGNOSIS
fever under evaluation ? Dengue
INVESTIGATIONS :
29/03/2022
Hemogram
HB- 13.4, TLC-8300, PLT - 1.42 lakhs
LFT :
DB - 0.58, IB-0.17, SGOT - 66, SGOT - 64, ALT -223,
TP- 5.1, G - 3.2, A/G - 1.73.
RFT
Sr urea - 10, Creatinine - 0.9,
Na/k/CL - 124/3.5/95
Dengue
NS1, IgM, IgG- negative.
ECG
2D ECHO
Chest X ray
Diagnosis - VIRAL PYREXIA
TREATMENT
1.IVF NS, RL, DNS @ 100ml /hr
2.Inj PAN 40 mg po/od
3.Inj zofer 4mg IV bd
4. Inj NEOMOL IV SOS
5. TAB DOLO 650 PO/ QID
6. TAB ULTRACET PO/BD.
30/03/2022 :
- Get link
- X
- Other Apps