66Y with SOB and Cough
- Get link
- X
- Other Apps
This is online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CONSENT AND DE-IDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whatsoever.
2019-patient had cough ,came to our hospital was diagnosed as pulmonary tuberculosis and was on medication for 6months anti tubercular therapy
12th DECEMBER 2021-patient had complaints burning pain,indigestion,loss of appetite ,on endoscopy it showed MUlTIPLE ESOPHAGEAL ULCERS
October 19th ,2022- patient came to our hospital with sob ,fever,cough expectoration and was diagnosed as viral pneumonia with CKD with post viral myalgia
Daily routine: 66M farmer by occupation but stopped his occupation due to debts.He wakes up daily at 7am then has chai and 10:00 am has rice and dal ,talks to his neighbours.At 12:00 pm has rice ,watches tv 8pm has rice and at 9:00pm goes to sleep.No change in daily routine. Sleep was disturbed since 3days due to SOB
Patient came with
c/o difficulty breathing since 2days (mmrc grade2)
C/o cough which is productive,scanty, whitish in colour and non blood stained
C/o bilateral pedal edema ,extending upto feet since 1year which is on /off
Patient was apparently asymptomatic 3days back ,then he developed fever which Is high grade,continous associated with chills and rigors ,relieved after taking medicine
Then he developed SOB which was sudden in onset and gradually progressive which aggravates on walking ,present even during rest
K/c/o CKD since 6months (on conservative management)
H/o TB 5years back
H/o viral pneumonia 1year back
N/kc/o HTN ,DM,thyroid,epilepsy,asthma
O/E:
GENERAL EXAMINATION
Pt is c/c/c
Afebrile on touch
PR:70 bpm
BP:130/70 mm hg
RR:26 cpm
GRBS:106mg/dl
Pallor present
Clubbing present
B/L pedal edema(pitting type) present
No Icterus,cyanosis, lymphadenopathy.
SYSTEMIC EXAMINATION
Respiratory system:
Inspection:
Tracheal deviation to right.
Chest bilaterally symmetrical
Type of respiration: Abdomino thoracic.
No dilated veins,pulsations,scars, sinuses.
No drooping of shoulder.
Palpation:
Tracheal deviation to right
Apex beat- 5th intercoastal space,medial to midclavicular line.
Tenderness over chestwall- absent.
Vocal fremitus- Mammary,Infra Axillary and Infrascapular- Decreased on both sides.
Percussion:
Dull note on left Inframammary,infraaxillary and infrascapular areas
Auscultation:
Dyspnea+
Wheeze in left inframammary area and bilateral infrascapular area ,crepts+
Tubular breath sounds heard
Ronchi+
Cardiovascular system:
Inspection : no visible pulsation , no visible apex beat , no visible scars.
Palpation: all pulses felt , apex beat felt.
Percussion: heart borders normal.
Auscultation:
Mitral area, tricuspid area, pulmonary area, aortic area- S1,S2 heard.
P/A:Soft ,Non-tender
CNS:
HMF-Intact
Memory -recent and remote:Intact
Speech-Normal
Cranial Nerves -Normal
Motor Examination-
Tone. UL. N. N
LL. N. N
Imaginary Pillow sign
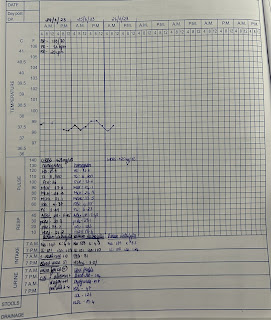
Investigations:
20/5/23
DIAGNOSIS:
Acute on chronic Bronchitis with metabolic acidosis (HAGMA) with cervical spondylosis with AKI on CKD(stage 4) k/c/o CKD since 6 months with PTB 5 years back
Follow up:
22/5/23
Admission date: 20/5/23
S
No fever spikes
Stools not passed today
O
Pt is conscious, Coherent and cooperative
BP - 100/60 mm hg
PR - 70 bpm
SPO2: 96% ON RA
RR: 16 cpm
CVS: S1S2 + , NO MURMURS
RS: BAE+ , Bronchial breath sounds heard in B/L Infraclavicular areas with grunting
B/L ISA crepts present
CNS-NFND
GCS E4 V5 M6
P/A: SOFT, TENDERNESS in Rt.Hypochondrium
I/O:2800ml/1300ml
GRBS: 78MG/DL
A
PNEUMONIA secondary to ?? Bacterial ??TB with metabolic acidosis (HAGMA) with cervical spondylosis with AKI on CKD(stage 4) k/c/o CKD since 6 months with PTB 5 years back
P
1.INJ.AUGMENTIN 1.2GM IV/BD
2.TAB.AZITHROMYCIN 500MG PO/OD
3.INJ.PAN 40MG IV/OD
4.IV FLUIDS NS@ Urine output+30ml/hr
5.TAB.NODOSIS 500MG PO/BD
6.TAB.OROFER-XT PO/OD
7.TAB.SHELCAL-CT PO/OD
8.Nebulization with budecort - 12 th hrly
Duolin -6 th hrly
9.Oxygen support if spo2 <92%
10. Strict I/O charting
11.Vitals monitoring 2nd hrly.
23/5/23
S
Two fever spikes
Stools passed today
O
Pt is conscious, Coherent and cooperative
BP - 120/70 mm hg
PR - 90 bpm
SPO2: 99% ON RA
RR: 24 cpm
CVS: S1S2 + , NO MURMURS
RS: BAE+ , Bronchial breath sounds heard crepts present in Right mammary,IAA,ISA
Crepts present in left mammary
CNS-NFND
GCS E4 V5 M6
P/A: SOFT, TENDERNESS in umbilicus and Rt.Hypochondrium
I/O:2500ml/2000ml
GRBS: 78MG/DL
A
Acute on chronic Bronchitis with metabolic acidosis (HAGMA) with cervical spondylosis with AKI on CKD(stage 4) k/c/o CKD since 6 months with PTB 5 years back
P
1.INJ.AUGMENTIN 1.2GM IV/BD
2.TAB.AZITHROMYCIN 500MG PO/OD
3.INJ.PAN 40MG IV/OD
4.IV FLUIDS NS@ 50ml/hr
5.TAB.DOLO 650mg PO/SOS
6.TAB.NODOSIS 500MG PO/BD
7.TAB.OROFER-XT PO/OD
8.TAB.SHELCAL-CT PO/OD
9.Nebulization with budecort - 12 th hrly
Duolin -6 th hrly
10.Oxygen support if spo2 <92%
11. Strict I/O charting
12.Vitals monitoring 2nd hrly.
24/5/23
S
Fever spikes present
Stools passed
O
Pt is conscious, Coherent and cooperative
BP - 100/70 mm hg
PR - 90 bpm
SPO2: 99% ON RA
RR: 26 cpm
CVS: S1S2 + , NO MURMURS
RS: BAE+ , NVBS
CNS-NFND
GCS E4 V5 M6
P/A: SOFT, NON TENDER
I/O:2400ml/2300ml
A
?BILATERAL COMMUNITY ACQUIRED PNEUMONIA secondary to ?? Bacterial ??TB ?Acute on chronic bronchitis with metabolic acidosis (HAGMA) with cervical spondylosis with AKI on CKD(stage 4) k/c/o CKD since 6 months with PTB 5 years back
P
1.INJ.AUGMENTIN 1.2GM IV/BD
2.TAB.AZITHROMYCIN 500MG PO/OD
3.INJ.PAN 40MG IV/OD
4.IV FLUIDS NS@ 50ml/hr
5.TAB.DOLO 650mg PO/SOS
6.TAB.NODOSIS 500MG PO/BD
7.TAB.OROFER-XT PO/BD
8.TAB.SHELCAL-CT PO/OD
9.Nebulization with budecort - 12 th hrly
Duolin -6 th hrly
10.Syp.Cremaffin 10ml po/hs
11.Oxygen support if spo2 <92%
12 Strict I/O charting
13.Vitals monitoring 2nd hrly.
25/5/23
S
Fever spike present
Stools passed
O
Pt is conscious, Coherent and cooperative
BP - 110/70 mm hg
PR - 94 bpm
SPO2: 98% ON RA
RR: 22 cpm
CVS: S1S2 + , NO MURMURS
RS:NVBS.
Fine crepts present in left Infrascapular and Infraaxillary area
CNS-NFND
GCS E4 V5 M6
P/A: SOFT, NON TENDER
I/O:2000ml/1700ml
GRBS-80 mg/dl
A
?BILATERAL COMMUNITY ACQUIRED PNEUMONIA secondary to ?? Bacterial ??TB ?Acute on chronic bronchitis with metabolic acidosis (HAGMA) with cervical spondylosis with AKI on CKD(stage 4) k/c/o CKD secondary to ?NSAID abuse since 6 months with PTB 5 years back
P
1.INJ.AUGMENTIN 1.2GM IV/BD
2.TAB.AZITHROMYCIN 500MG PO/OD
3.INJ.PAN 40MG IV/OD
4.IV FLUIDS NS@ 50ml/hr
5.TAB.DOLO 650mg PO/SOS
6.TAB.NODOSIS 500MG PO/BD
7.TAB.OROFER-XT PO/BD
8.TAB.SHELCAL-CT PO/OD
9.Nebulization with budecort - 12 th hrly
Duolin -6 th hrly
10.Syp.Cremaffin 15ml po/hs
11.Oxygen support if spo2 <92%
12 Strict I/O charting
13.Vitals monitoring 2nd hrly.
26/5/23
S
No Fever spikes
Stools passed
O
Pt is conscious, Coherent and cooperative
BP - 110/70 mm hg
PR - 90 bpm
SPO2: 98% ON RA
RR: 20 cpm
CVS: S1S2 + , NO MURMURS
RS:NVBS.
Fine crepts present in both right and left Inframammary and Infraaxillary areas
CNS-NFND
GCS E4 V5 M6
P/A: SOFT, NON TENDER
I/O:2000ml/1700ml
GRBS-80 mg/dl
A
?BILATERAL COMMUNITY ACQUIRED PNEUMONIA secondary to ?? Bacterial ??TB ?Acute on chronic bronchitis with metabolic acidosis (HAGMA) with cervical spondylosis with AKI on CKD(stage 4) k/c/o CKD secondary to ?NSAID abuse since 6 months with PTB 5 years back
P
1.TAB.AZITHROMYCIN 500MG PO/OD
2.TAB.DOLO 650mg PO/SOS
3.TAB.NODOSIS 500MG PO/BD
4.TAB.OROFER-XT PO/BD
5.TAB.SHELCAL-CT PO/OD
6.Nebulization with budecort - 12 th hrly
Duolin -6 th hrly
7.Syp.Cremaffin 15ml po/hs
8.Oxygen support if spo2 <92%
9. Strict I/O charting
10.Vitals monitoring 2nd hrly.
27/5/23
S
Fever spike present
Stools passed
O
Pt is conscious, Coherent and cooperative
BP - 110/70 mm hg
PR - 94 bpm
SPO2: 98% ON RA
RR: 22 cpm
CVS: S1S2 + , NO MURMURS
RS:NVBS.
Fine crepts present in left Infrascapular and Infraaxillary area
CNS-NFND
GCS E4 V5 M6
P/A: SOFT, NON TENDER
I/O:2000ml/1700ml
GRBS-80 mg/dl
A
?BILATERAL COMMUNITY ACQUIRED PNEUMONIA secondary to ?? Bacterial ??TB ?Acute on chronic bronchitis with metabolic acidosis (HAGMA) with cervical spondylosis with AKI on CKD(stage 4) k/c/o CKD secondary to ?NSAID abuse since 6 months with PTB 5 years back
P
1.INJ.AUGMENTIN 1.2GM IV/BD
2.TAB.AZITHROMYCIN 500MG PO/OD
3.INJ.PAN 40MG IV/OD
4.IV FLUIDS NS@ 50ml/hr
5.TAB.DOLO 650mg PO/SOS
6.TAB.NODOSIS 500MG PO/BD
7.TAB.OROFER-XT PO/BD
8.TAB.SHELCAL-CT PO/OD
9.Nebulization with budecort - 12 th hrly
Duolin -6 th hrly
10.Syp.Cremaffin 15ml po/hs
11.Oxygen support if spo2 <92%
12 Strict I/O charting
13.Vitals monitoring 2nd hrly.
66Y old male with c/o difficulty in breathing, cough since 2 days and bilateral pedal edema was investigated further Sputum for C/s and gram staining and AFB staining were done and found out to be Negative.
Popular posts from this blog
22Y M WITH INVOLUNTARY MOVEMENTS OF HEAD AND UPPER LIMBS
90Yr Male with Altered sensorium
Internship Assessment
- Get link
- X
- Other Apps