75 YEAR MALE ;RIGHT HEMIPARESIS
A 75 year old Male,Farmer by occupation (stopped working 5 years ago) from Nalgonda was brought to casualty by his son in an unresponsive state and altered sensorium since 3 days.
Daily routine and lifestyle:
He initially used to work in band ( plays music during the functions) 15 years back
His routine is active lifestyle
With all his works being done by him and rides his bike
And switched his job to farmer as he's getting aged and has to look after their farm
During this period he had increased consumption of alcohol ( frequency- 3-4times/week)
He was asked to stop working by his sons 2 years back as he is aging
He started staying at his sons house but used to maintain his active lifestyle by doing household chores ,getting groceries,cleans and maintains nearby dargah
HISTORY OF PRESENT ILLNESS -
Patient was apparently asymptomatic 10 years ago, when he had a h/o fall and had an IT fracture for which he was managed conservatively.
Patient had SOB ? Asthma 2 years ago for which he was managed conservatively and was advised to stopped smoking and alcohol intake
14/6/23-
Patient was drowsy and was not having food
After 2- 3hours patient developed left upper and lower limb weakness with deviation of mouth
But was able to move his limbs and recognise attenders
Later was taken to gollagudem hospital was given symptomatic management
Patient is conscious ,irritable
And was referred to nalgonda hospital
18/6/23 - patient had increased drowsiness and altered sensorium with decreased responsiveness to commands
( patient was given librium )
19/6/23 -
In view of persisting altered sensorium ct brain was done In the next two days, patient showed slight improvement in his symptoms
Recognising attenders ,movement of limbs +
On Friday 24.6.23 night patient had tachepnoeaa and decreased saturations and increased drowsiness, and hence later he came to our hospital on 24.6.23 as they were advised that the patient is in need of mechanical ventilation
Patient presently has a history of alcohol intake 8 days ago, and he developed craving for alcohol 3 days ago and was in agitated state, irritable and also self talk.
Patient has no H/O cough, cold, loose stools, vomitings, burning micturition.
PAST HISTORY:
No similar complaints in the past
No H/o Type II DM , Hypertension, TB, CAD , Epilepsy and Thyroid disorders
PERSONAL HISTORY:-
Diet: Mixed
Appetite: Normal
Sleep: Adequate
Bowel & bladder: Regular
Patient has h/o beedi smoking for about 10 years (2-3 beedis/ day), stopped 2 years ago and presently has on and off history of beedi smoking since 2 years
Patient was a chronic alcoholic for about 10 years. Stopped 2 years ago but has a h/o on and off alcohol consumption.
Last intake - 8 days ago
No allergies
FAMILY HISTORY:
No significant family history
GENERAL EXAMINATION:
Patient is in altered sensorium
Moderately built, well nourished
No pallor/icterus/cyanosis/clubbing/Generalized lymphadenopathy/pedal edema
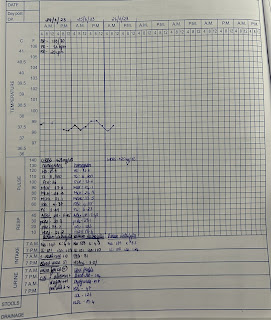
VITALS:
Temp: 99.4 F
PR: 93 bpm
RR: 34cpm
BP: 130/80mmHg
Spo2: 99%@RA
GRBS: 127mg/dl
SYSTEMIC EXAMINATION:
CVS: S1 S2 heard, No murmurs
RS: BAE+
P/A: soft, non tender
A soft palpable mass is present over epigastrium
No engorged veins, scars or sinuses
1. Autonomic function: Normal
2. CNS examination:
GCS- E1V1M5
Pupils -B/L NSRL
MOTOR SYSTEM :
Right Left
Bulk: N. N
Tone: Right Left
UL. N N
LL. N. N
Deep tendon reflexes:
Biceps: +2 +2
Triceps: +2 +2
Supinator:. +2 +2
Knee: - -
Ankle: +1 +1
Plantar: - -
Sensory:
CRANIAL NERVES : Couldn't be assessed as the patient is in altered sensorium.
Pulmonology referral-
1. Consider intubation i/v/o low GCS
2. CST
PROVISIONAL DIAGNOSIS -
Altered sensorium secondary to ? Acute ischemic stroke ? Alcohol withdrawal with Type II Respiratory failure secondary to ? Pulmonary edema ? Aspiration Pneumonia with B/L Hydrocele with Right LL IT fracture 10 years ago.
Investigations -24/6/23
ABG -
pH- 7.44
PO2- 65.9
PCO2- 28.6
HCO3- 19.1
Hb: 15.1 gm/dl
TLC: 15,200
Platelets :2.91
PBS:NC/NC with WBC leukocytosis
RBS - 132 mg/dl
Urea: 57
Creatinine: 1.1
Na: 138
K:4.8
Cl:98
Total bilirubin 0.89
Direct bilirubin 0.19
AST 27
ALT. 19
ALP. 128
Total protein 6.6
Albumin 3.58
A/G: 1.19
CUE: Albumin +
Sugar- nil
Ep cells - 2-3
Pus cells -2-4
HBsAG - negative
HCV- negative
HIV 1/2 -negative
ECG -
Chest X-Ray
USG abdomen -
USG - B/L INGUINO-SCROTAL REGION -
CT Brain - plain
Impression-
1. Hypodensity involving right temporo parietal region - P/O infarct
2. White matter and periventricular changes are noted
3. SVIC -1
4. Age related atrophy
2D ECHO -
Concetric LVH (1.42 cms)
No RWMA
Paradoxical IVS
Trivial AR +/PR+
NO MR
Sclerotic AV , No AS/MS
EF - 60%
RSVP - 36 mm hg
Good IV systolic function, diastolic dysfunction+
No PA/ PAE
IVC - 0.9 cms (collapsing)
Treatment -
1. IVF NS , 5D AT 50ML / HR
2. Head end elevation
3. Ryles feed 200ml milk + protein powder 4th hourly and 100 ml water 2nd hourly
4. O2 support to maintain saturation above 92%
5. Inj. PIPTAZ 4.5 g IV/ Stat f/b Inj. PIPTAZ 4.5 g IV/ TID
6. Inj. Clindamycin 600 mg IV / BD
7. Inj. Pantop IV/OD/ BBF
8. Inj. Thiamine 200 mg + 100ml NS IV/OD
9. Tab. Ecosprin - AV 75/20/ RT/ HS
10. Tab PCM 650 mg RT/ SOS (>100F)
11. Nebulization Budecort and Ipravent 6th hourly. Mucomist - 4th hourly
12. Chest physiotherapy, postural drainage
13. Suctioning 4th hourly
14. DVT stockings and position change 2nd hourly
15. Strict I/O charting